- Home
- Junior Research Groups
- Ultrafast Fiber Lasers
- Research results
- Light Instead of a Needle and Thread
Light Instead of a Needle and Thread
17.05.2021
Welding with ultrashort laser pulses: researchers are working on a gentle method to rejoin tissue
To reconnect organs and tissues as naturally as possible after a surgical procedure and to restore function quickly, lasers are increasingly proving to be a gentle and effective alternative. Established methods of resealing wounds by suturing, stapling, or gluing, while well developed, are not a panacea. For example, glues, once applied, do not allow correction of wound closure, while metal staples, for example, do not form a watertight bond, which can lead to inflammation.
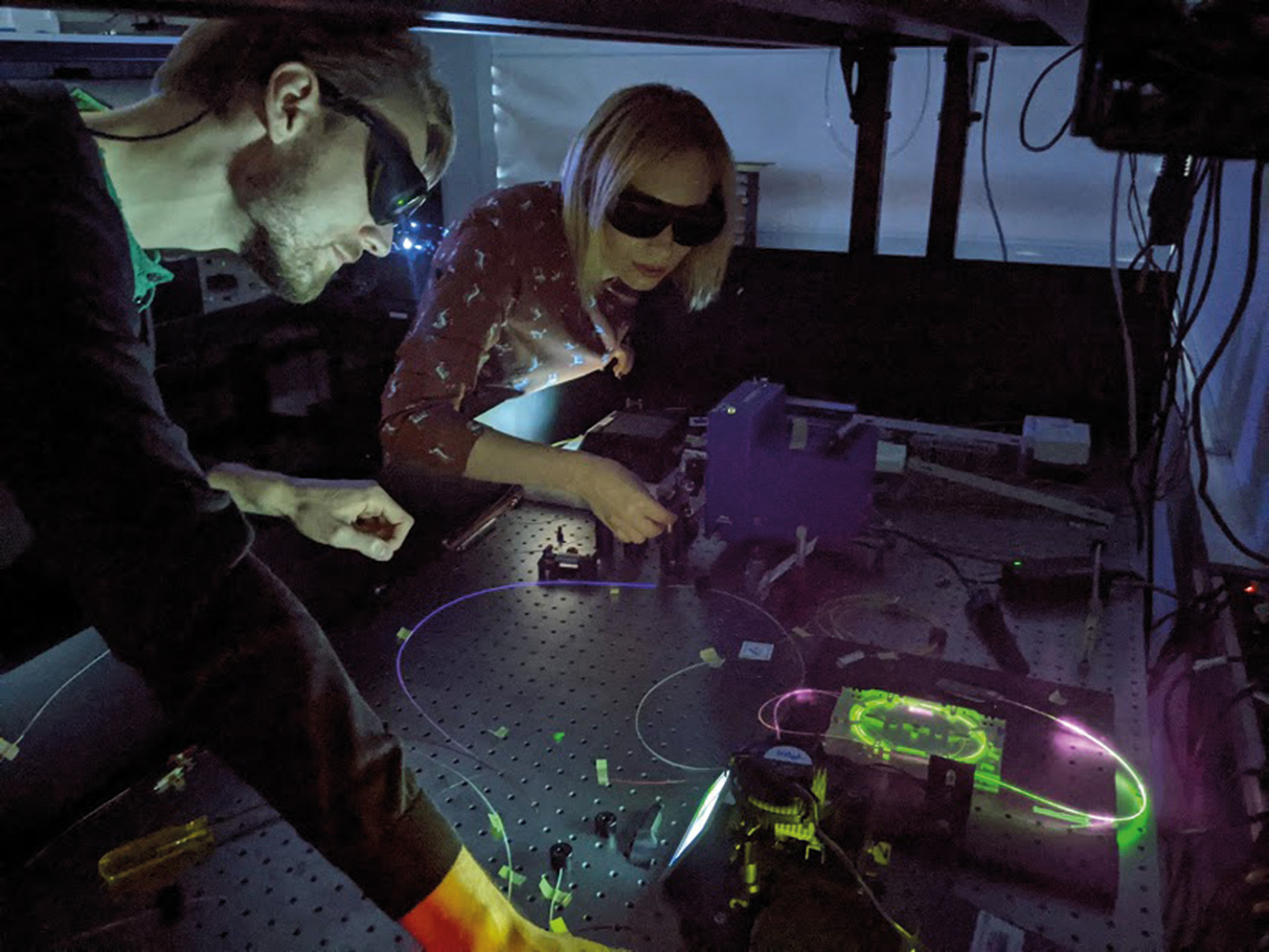
Maria Chernysheva, head of the junior research group “Ultra Short Pulse Fiber Lasers”, together with a team from the British Aston Medical School, has now developed a multifunctional optical fiber probe that can be used to reliably connect biological tissue. Using an ultrafast fiber laser, the researchers succeeded in welding the walls of dissected chicken hearts together in such a way that a tensile bond corresponding to the native tissue was created. The researchers monitored the welding process using fluorescence spectroscopy, which detects the biochemical composition of the tissue. “We came up with this idea quite spontaneously,” Maria Chernysheva reports. “During an experiment on laser ablation of cardiac tissue, we noticed that the fluorescence spectrum of the tissue during laser irradiation behaved differently than we expected for certain radiation parameters.” When they examined the spectrum, the researchers concluded that the increase in characteristic peaks of elastin, collagen, and methemoglobin indicated the onset of welding. Guided by fluorescence spectroscopy, they varied laser power, pulse packet duration, and exposure rate and eventually found the most effective method. Compared to conventional mode-locked operation, this enables tissue to be welded more gently and at the same time more deeply.
Faster healing, Fewer complications
“Compared to conventional suturing, laser welding is potentially less traumatic as well as easier and faster for surgeons to perform,” explains Maria Chernysheva. “Healing is accelerated. The wound is immediately tightly closed, and the risk of postoperative complications decreases.” Foreign body reactions are thus avoided; the risk of necrosis – a death of tissue – at the edges is minimized, as is the formation of a large scar.
In a next step, the researchers now want to extend their approach to minimally invasive surgery to other biological tissues and explore laser welding of tissue for in vivo use. A long-term study on animal models will show how laser welding affects the dynamics of wound healing.