- Home
- Research
- Spectroscopy and Imaging
- Research results
- New Approach to Early Detection of Severe COVID-19
New Approach to Early Detection of Severe COVID-19
05.09.2023
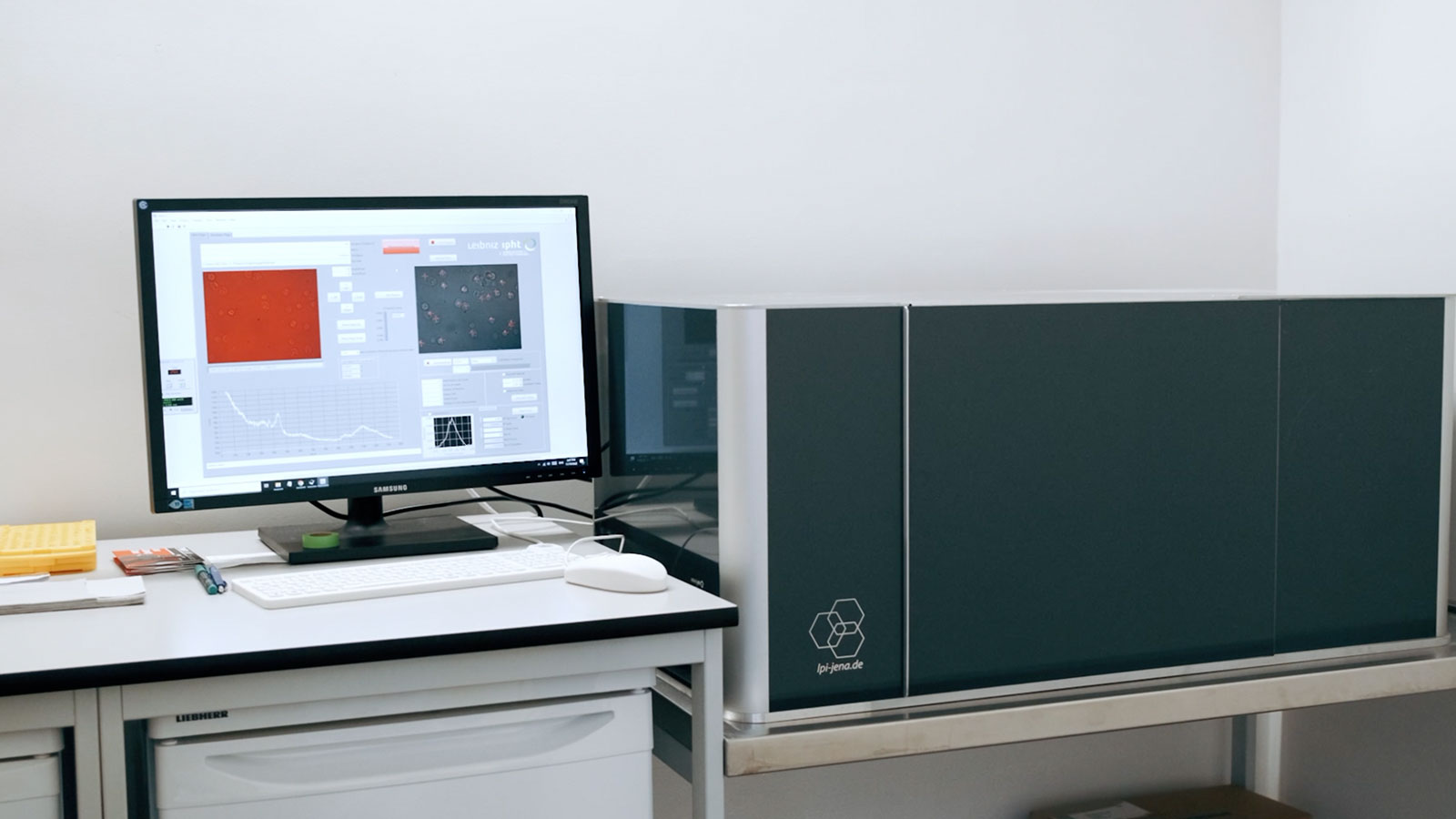
An interdisciplinary team of researchers at LPI is investigating the extent to which spectroscopic methods are suitable for predicting the further course of a corona disease at an early stage. They examine infected white blood cells with a high-throughput Raman system in order to analyze the immune response.
The symptoms of a COVID-19 infection can vary widely, ranging from mild respiratory symptoms to life-threatening lung dysfunction. Already at an early stage of the disease, conclusions about the further course of the disease could be drawn on the basis of the immune response. As part of joint projects and clinical studies, scientists from the Leibniz IPHT together with colleagues from the Jena University hospital investigate the potential use of photonic technologies for the early detection of a severe COVID-19 course of disease. The findings could help to better understand and predict the course of the disease and to take life-saving measures at an early stage.
For their studies, the researchers used Raman spectroscopic methods to detect changes in the molecular composition of white blood cells. To do this, they infected neutrophil granulocytes in the laboratory with the corona virus and stimulated the immune response by adding inflammatory messenger substances. Neutrophil granulocytes are the most common type of white blood cells. They respond rapidly to inflammation and infection by absorbing and destroying bacteria or other pathogens. Using High-Throughput Screening Raman Spectroscopy (HTS-RS), the researchers examined the white blood cells at different time intervals. The spectra obtained in this way were then analyzed using machine-based learning algorithms.
Significant changes in the Raman spectroscopic fingerprint of the infected immune cells could be observed and distinguished from each other after three and after 24 hours. The measurement data indicate a phenotypic change of neutrophil granulocytes caused by an increased production of cytokines. An increased release of this messenger substance could be biochemically detected in the cells infected with SARS-CoV-2 after three hours. After a further 21 hours, the production of the proteins responsible for the immune response had increased significantly.
The Raman data can therefore not only be used to distinguish whether a cell is infected or not. The conclusion that the Raman signature correlates with the cytokine level is also obvious. Based on these findings, the methodology and data analysis will be further trained and improved by using artificial intelligence. In the long term, this may result in a new diagnostic tool for the early detection of a severe COVID-19 course of disease, which could be an alternative or complement to existing biochemical methods.
